Neurodegenerative diseases can damage different parts of the nervous system, including the brain. This may lead to problems with thinking, memory, and/or movement. Examples include Alzheimer’s disease (AD), multiple sclerosis (MS), and Parkinson’s disease (PD). These diseases tend to happen late in life. There are few effective treatments.
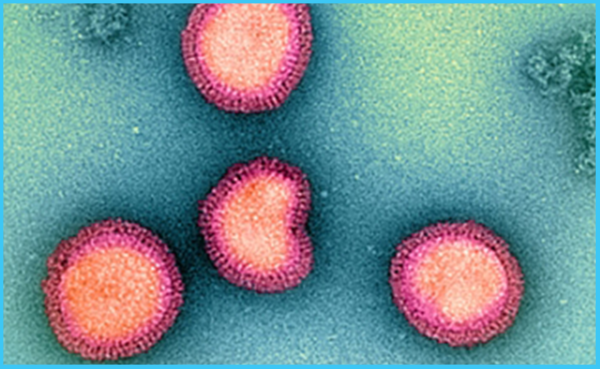
Previous findings have suggested that viruses may play a role in certain neurodegenerative diseases. For example, a recent study found a link between Epstein-Barr virus infection and the risk of MS. There are concerns about cognitive impacts from SARS-CoV-2, which causes COVID-19.
A research team led by Drs. Mike Nalls, Kristin Levine, and Hampton Leonard of NIH’s Center for Alzheimer’s and Related Dementias more generally examined links between viruses and neurodegenerative diseases. To do so, they analyzed data from the FinnGen project. This is a biomedical data repository, or biobank, from over 300,000 people in Finland. The team searched the biobank for people who had been diagnosed with one of six different conditions: AD, amyotrophic lateral sclerosis, generalized dementia, vascular dementia, PD, and MS. They then checked how many had been hospitalized for a viral illness before. To confirm their findings, they looked for the same associations in the UK Biobank, which contains data from almost 500,000 people in the United Kingdom. Results appeared in Neuron on Jan. 19, 2023.
The researchers found 45 associations between viruses and neurodegenerative diseases in FinnGen. Of these, 22 also appeared in the UK Biobank. The strongest association was between viral encephalitis — brain inflammation caused by a virus — and AD. A person with viral encephalitis in the FinnGen database was 30 times as likely to be diagnosed with AD as someone without encephalitis. Results were similar in the UK Biobank; people with viral encephalitis were 22 times more likely to develop AD than those without.
The team also found, in FinnGen, the association between the Epstein-Barr virus and MS that was described before. The association wasn’t seen in the UK Biobank, but this may reflect how the different biobanks use hospital diagnostic codes; Epstein-Barr viruses are common and so often not noted.
Influenza with pneumonia was associated with all neurodegenerative diseases except MS. The researchers only included cases of influenza severe enough to need hospitalization in the study. Thus, these associations only apply to the most severe cases of influenza.
FinnGen contains data on the same people over time. The team used this to examine how the associations depended on the time since infection. They found that some viral infections were associated with an increased risk of neurodegenerative disease as much as 15 years later.
The researchers note that vaccines exist for some of the viruses they identified. These include influenza, varicella zoster (which causes chickenpox and shingles), and certain pneumonia-causing viruses. Vaccination might thus reduce some of the risks of the conditions they examined.
“The results of this study provide researchers with several new critical pieces of the neurodegenerative disorder puzzle,” Nalls says. “In the future, we plan to use the latest data science tools to not only find more pieces but also help researchers understand how those pieces, including genes and other risk factors, fit together.”